Understanding the Dopamine Hypothesis of Schizophrenia: A Comprehensive Guide to Neurochemical Insights and Behavioral Health Strategies
Schizophrenia remains one of the most challenging mental health conditions to understand and treat effectively. Central to its neurobiological framework is the dopamine hypothesis of schizophrenia, which postulates that dysregulated dopamine activity plays a critical role in the manifestation of psychotic symptoms. This article dives deep into the origins, scientific evidence, clinical implications, and current treatment approaches associated with this hypothesis, highlighting how behavioral health services at institutions like behavioralhealth2000.com are leveraging these insights to enhance patient care and outcomes.
Introduction to the Dopamine Hypothesis of Schizophrenia
The dopamine hypothesis of schizophrenia originated in the mid-20th century when researchers observed that drugs influencing dopamine levels could alter psychotic symptoms. The hypothesis suggests that an overactivity of dopamine transmission in particular brain pathways contributes to the characteristic symptoms of schizophrenia, including hallucinations, delusions, and disorganized thinking. Understanding this connection has spurred numerous advances in both pharmacological and behavioral treatments, creating a more nuanced approach to managing this complex disorder.
The Neurobiology of Schizophrenia and Dopamine's Role
Schizophrenia is a multifaceted neuropsychiatric disorder involving alterations in multiple brain regions and neurotransmitter systems. However, dopamine plays a pivotal role in modulating neural circuits responsible for perception, cognition, and emotional regulation. The neurobiology centers around two major dopaminergic pathways:
- Mesolimbic Pathway: Hyperactivity in this pathway is associated with positive symptoms such as hallucinations and delusions.
- Mesocortical Pathway: Hypoactivity here has been linked to negative symptoms like social withdrawal and cognitive deficits.
This dichotomy underscores the importance of balanced dopamine activity for healthy mental functioning. Disruptions in these pathways resonate strongly with symptom severity, guiding targeted therapies.
Historical Development and Scientific Evidence
The origins of the dopamine hypothesis trace back to the discovery that the antipsychotic medications of the 1950s, notably chlorpromazine, primarily function as dopamine antagonists. This led researchers to theorize that excess dopamine activity contributed to psychotic symptoms. Over the subsequent decades, scientific investigations have provided robust evidence supporting this hypothesis:
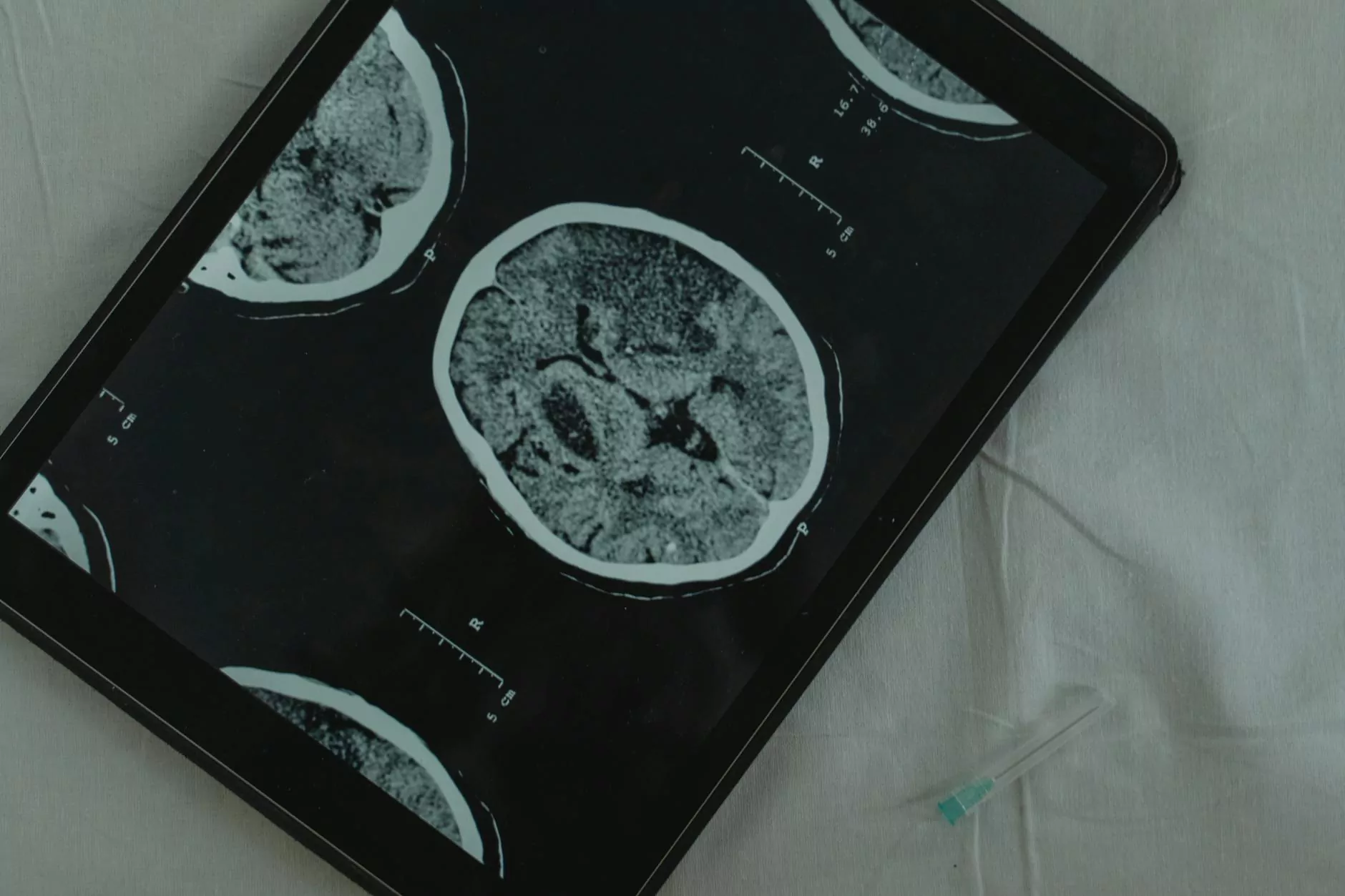
- Neuroimaging Studies: PET and SPECT scans have demonstrated increased dopamine synthesis and release in patients with schizophrenia.
- Pharmacological Data: Dopamine agonists can induce psychosis-like symptoms, while antagonists mitigate positive symptoms.
- Genetic Research: Variations in genes controlling dopamine regulation have been linked to a heightened risk of schizophrenia.
However, it's important to recognize that the dopamine hypothesis is not the sole explanation; it forms part of a broader neurochemical and genetic model necessary to understanding the full spectrum of the disorder.
Implications for Treatment Strategies in Mental Health
The insights derived from the dopamine hypothesis have profoundly influenced the development of antipsychotic medications. Traditional antipsychotics, such as haloperidol, primarily function as dopamine D2 receptor antagonists, effectively reducing positive symptoms. Conversely, atypical antipsychotics target multiple neurotransmitter systems, offering improved efficacy for negative and cognitive symptoms.
Behavioral health professionals now combine pharmacological treatments with evidence-based psychotherapies—like cognitive-behavioral therapy (CBT) and social skills training—to address the neurochemical imbalances within a holistic framework.
Furthermore, continual research into dopamine's intricate functions has opened pathways for novel treatments, including dopamine partial agonists and agents targeting specific receptor subtypes, heralding a new era in personalized mental health care.
The Role of Behavioral Health Services in Managing Dopaminergic Dysregulation
While medications play a vital role, behavioral health services are essential for fostering environmental, psychological, and social factors that influence disease trajectory. At behavioralhealth2000.com, tailored programs focus on:
- Patient Education: Explaining the neurochemical basis of schizophrenia to empower individuals and families.
- Cognitive Therapies: Enhancing coping strategies for managing symptoms related to neurochemical imbalances.
- Monitoring and Compliance: Ensuring adherence to medication regimens that target dopaminergic pathways.
- Community Support: Creating social environments conducive to stabilization and recovery.
Implementing these strategies results in improved quality of life and a reduction in relapse rates, emphasizing the synergy between neurochemical understanding and behavioral interventions.
Innovations and Future Directions in Understanding the Dopamine Hypothesis
The scientific community continues to refine its understanding of dopamine's role in schizophrenia, exploring intersections with other neurotransmitter systems such as glutamate and serotonin. Emerging research suggests that:
- Neuroplasticity: Dopamine dysregulation impacts brain circuit adaptability, opening avenues for neurorestorative therapies.
- Genomics and Precision Medicine: Genetic profiles may predict individual responses to dopaminergic treatments.
- Novel Pharmacological Agents: Drugs targeting specific dopamine receptor subtypes or modulating downstream signaling pathways.
These advances aim to develop more effective, personalized interventions that mitigate side effects and target the core neurochemical imbalances in schizophrenia.
Conclusion: Integrating Neurochemical Insights with Holistic Care
The dopamine hypothesis of schizophrenia remains a cornerstone of neuropsychiatric research, offering invaluable insights into the biological underpinnings of psychosis. Its influence extends beyond pharmacology, informing behavioral health strategies that aim to restore balance in brain chemistry while supporting psychosocial well-being.
Effective management of schizophrenia requires a comprehensive, multidisciplinary approach — combining evidence-based medications, therapeutic interventions, and community support—ultimately improving patient outcomes and quality of life. As research progresses, hope for more precise and less invasive treatments grows, promising a brighter future for individuals affected by this complex disorder.
About BehavioralHealth2000.com
At behavioralhealth2000.com, our mission is to provide innovative and compassionate mental health and counseling services. We are dedicated to integrating the latest neurobiological research, including understandings like the dopamine hypothesis of schizophrenia, into personalized treatment plans that foster healing, resilience, and growth.









